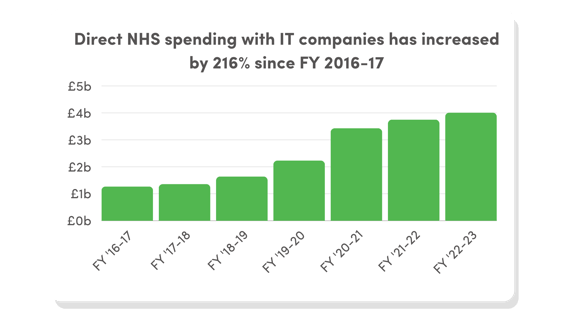
Amidst rapid digitisation, NHS spending with technology companies has ballooned by 216% since FY16/17.
In an era of unprecedented challenges - patient waiting times, demographic shifts, budget restrictions, a mental health crisis etc. - new technologies promise to provide solutions to an ever-growing list of demands.
The need to build effective business cases for these new technologies and deploy systems effectively and efficiently has never been greater.
In this guest blog, Alan Brown, Managing Director at Apira - one of this year's 200 fastest-growing tech suppliers - shares his best practice advice for NHS trusts on how to build out a business case and deploy systems for a digital healthcare future.
Skip ahead to read about:
Alan Brown, Managing Director, Apira
Apira ranked 35th in Tussell and techUK's 2023 Tech200 list of the fastest-growing technology companies in the UK public sector. One of only a few companies to enter the Tech200 twice in three years, their long and rapidly expanding list of NHS clients speaks to their trust and expertise in the healthtech sector. Apira specialise in helping healthcare providers realise their digital journeys. They are experts in procurement, deployment and implementation, working across a range of technologies and services such as radiology information systems, electronic patient records and electronic document management.
Introduction
In the dynamic world of healthcare, the need for technological transformation is no longer an option but a crucial imperative. With over two decades of experience in business-focused IT service delivery, particularly in the healthcare sector, I have witnessed the challenges faced by NHS Trusts and the transformative potential technology holds.
In this article, we will explore best practices for NHS Trusts when building a business case and preparing to deploy systems to address the pressing issues and embrace a digital future.
📃 Current challenges in healthcare
NHS Trusts grapple with numerous challenges that necessitate the adoption of new systems.
Inefficiencies, poor productivity, suboptimal patient and staff experiences, and the lack of timely access to crucial information are pressing concerns. Sharing information between different organisations and using data effectively for organisational management adds to the challenges faced by healthcare providers.
The integration of technology offers a pathway to address these challenges and introduces efficient healthcare delivery. A better flow of information between clinicians, support for patient pathways, workflow optimisation, and eliminating data entry duplication are key advantages. Additionally, providing patients with access to their own records empowers individuals and contributes to a patient-centric healthcare system.
🛠️ Building a business case: key considerations
When constructing a business case, NHS Trusts must meticulously evaluate several factors:
-
Identify Improvement Needs: Clearly define what needs improvement within the healthcare system.
-
Cost Evaluation: Understand the financial implications of the proposed system implementation, ensuring a comprehensive and realistic budget.
-
Articulate Benefits: Clearly articulate the benefits of the proposed system in a monetizable manner, showcasing the return on investment.
-
Stakeholder Involvement: Identify key stakeholders and involve them in the decision-making process to ensure broad support and representation.
-
Prioritisation Amidst Other Priorities: Develop strategies for effective project management and execution amidst competing priorities
📍 Strategies for inclusive decision-making
Involving healthcare professionals, administrators, and stakeholders in the decision-making process is paramount. Employing surveys, dedicated workshops, attending existing meetings, direct communication, and providing tangible materials for review fosters engagement and ensures diverse perspectives are considered.
🌐 Selecting and deploying appropriate systems
Selecting and deploying systems require a strategic approach:
-
Scope Evaluation: Define the scope of the system carefully, considering the balance between benefits and simplicity versus cost.
-
Involving the Right People: Identify the right stakeholders for system selection, acknowledging the potential time constraints to their involvement and addressing them proactively.
-
Decision-Making Criteria: Establish clear decision-making criteria and prioritise factors to guide the selection process effectively.
🚑 Mitigating risks during implementation
Mitigating risks during implementation is crucial for successful adoption of new systems. This involves establishing strong governance structures and delegated authority to ensure timely decision-making by the right individuals, including clinicians.
Assembling a diverse team with a mix of individuals familiar with Trust processes and experienced experts from specialised consultancies adds valuable expertise.
Moreover, recognising that going live is not the end of the programme emphasises the importance of ongoing optimisation to fully realise the system's potential and benefits.
🏥 Technology's role in patient outcomes
Technology, when effectively implemented, ensures the right information reaches the right person at the right time and place. It supports the patient journey by suggesting pathways and solutions while keeping clinicians in control.
💻 Ensuring proficiency in system usage
Ensuring healthcare professionals are proficient in using new systems involves a multifaceted approach:
-
Comprehensive Training: Provide comprehensive training, not just on the system itself, but on how it changes existing processes and workflows.
-
Accessible Support: Ensure readily accessible support for users to seek assistance when and where needed.
-
Testing and Familiarisation: Involve users in testing processes to ensure the system functions as intended and increase familiarity before the system goes live.
-
Seamless Access: Ensure easy and fast access to the system and to data that is not migrated.
🌅 Future outlook and preparation
As we look to the future, it's imperative for NHS Trusts to recognise that these technological systems are not mere optional investments but essential infrastructure for a modern health service. The notion of these systems being "affordable" must be replaced with an understanding that they are vital for delivering optimal care.
In conclusion, the integration of technology into healthcare is a journey that requires strategic planning, stakeholder engagement, and a commitment to ongoing improvement. By embracing these best practices, NHS Trusts can navigate the complexities of building a business case and deploying systems, paving the way for a digitally empowered healthcare future that benefits patients, staff, and taxpayers alike.
👇 Concluding remarks
The NHS technology market is one of the fastest growing public sector marketplaces.
In 2023, 29 of the 200 fastest growing public sector technologies companies (as identified in Tussell and techUK's Tech200) were found to provide healthtech products and services.
Rory's advice offers a framework for procurement and system implementation that straddles the full length of the procurement and technology onboarding process. His 'best practice' tips provide an effective solution to sustainable system deployment in a sector where digitisation is vital to patient outcomes.
Head to Tussell's Tech200 list to discover the fastest-growing technology companies in the public sector and how they can help your trust. Or, speak to the Tussell team to learn more about how a data driven approach to procurement could save you time and money in technology procurement and onboarding.



![[Gov] New Nav Bar, Solutions - DSIT citation v1, Rounded](https://www.tussell.com/hubfs/%5BGov%5D%20New%20Nav%20Bar%2c%20Solutions%20-%20DSIT%20citation%20v1%2c%20Rounded.png)
![New Nav Bar - New Tag [Gov]](https://www.tussell.com/hubfs/New%20Nav%20Bar%20-%20New%20Tag%20%5BGov%5D.png)

![[Gov] New Nav Bar, Insights - SS Report v1, Rounded](https://www.tussell.com/hubfs/%5BGov%5D%20New%20Nav%20Bar%2c%20Insights%20-%20SS%20Report%20v1%2c%20Rounded.png)